Middle East Respiratory Syndrome (MERS) is a disease caused by human coronaviruses (CoVs) that first emerged in the Middle East in 2012. In the past month, MERS has spread more rapidly, and claimed more lives than in the last two years. Understanding this dangerous disease, and the precautions needed to combat its spread is becoming increasingly important to global health security.
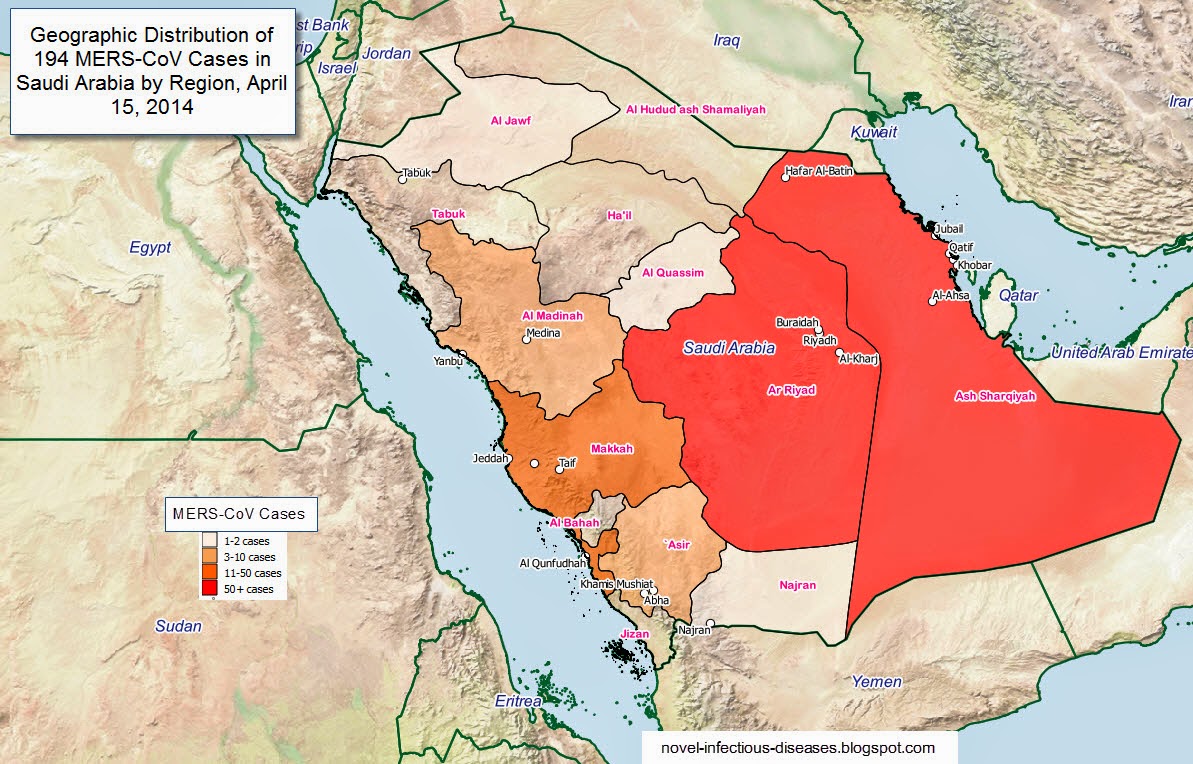
From September 2012 to the end of 2013, the WHO had been informed of 176 laboratory-confirmed cases of infection with MERS-CoV, including 74 deaths. As of May 28, 2014, 636 laboratory-confirmed cases of infection with MERS have officially been reported to WHO, including 193 deaths. May 2014 has been by far the worst month for the spread of MERS to date, with 375 confirmed cases and 100 deaths being reported to the WHO between April 26 and May 28 alone.
The first recorded incidences of MERS occurred in April 2012, when a group of 11 people, mostly healthcare workers, developed a severe lower respiratory infection of unknown cause in Zarga, Jordan. This was later linked to a 60 year old patient in Saudi Arabiawho died from an acute respiratory infection and renal failure in September. Clinical samples collected from this patient were used to identify and characterize MERS as a coronavirus.
Human coronaviruses cause a significant percentage of common colds worldwide. These viruses emerged from animal pathogens that crossed the species barrier, most of which originated in bats. CoVs have a high instance of genetic mutation that gives them an accelerated ability to adapt to different hosts. This was the case 10 years ago when Severe Acute Respiratory Disease (SARS), another CoV, emerged from horseshoe bats.

Contact between bats and humans is rare, so intermediary hosts are suspected to be involved in transmitting CoVs to humans. In the case of SARS, civet cats are thought to be responsible for the spread of SARS in China. Researchers have demonstrated that Camels may be responsible for MERS becoming transmissible to humans. Camels have been found by many studies to be positive for MERS, and viral RNA sequences obtained from camels have been found to be nearly identical to the human MERS strain.
Human to human transmission of the disease has been found in many areas. Clusters of MERS outbreaks have been found in Saudi Arabia, United Arab Emirates, Qatar, Oman, Jordan, Kuwait, Yemen, and Lebanon. More recently, cases have emerged in Algeria, Iran, and the United States. Travel related instances of the disease have also occurred in European countries such as France, the United Kingdom, Greece, and the Netherlands.
Individuals infected with MERS will develop symptoms between 2 and 14 days of being exposed. Symptons include fever, coughing, shortness of breath, and gastrointestinal distress. About 30% of those exposed to MERS have died, but most of these cases involved patients with existing underlying medical conditions.
The Public Health Agency of Canada considers the public health risk posed by MERS to be low at this time, but that this may change as new information arises. According to the WHO International Health Regulations Emergency Committee, the seriousness of MERS in regard to public health impact has increased.
The WHO is advising that health care workers and visitors in facilities that have suspected or confirmed MERS patients should be educated and refreshed on infection prevention and control measures, and recent travellers in the Middle East who develop severe acute respiratory infections should be tested for MERS. The WHO does not, however, suggest any trade or travel restrictions should be imposed at this time.